Choosing the proper contraception method can feel overwhelming when you’re bombarded with conflicting information online, outdated myths spread by well-meaning friends, and concerns about what’s actually safe for your body. You deserve clear, evidence-based answers about intrauterine devices (IUDs) from trusted gynecology professionals that help you make an informed decision without confusion.
Whether you’re considering your first long-term birth control option or want hassle-free contraception that fits your lifestyle, understanding IUDs empowers you to take control of your reproductive health with confidence.
What Is An IUD Device?
An intrauterine device represents one of the most effective forms of reversible birth control available today, offering you peace of mind without daily maintenance or frequent OBGYN visits for prescription refills.
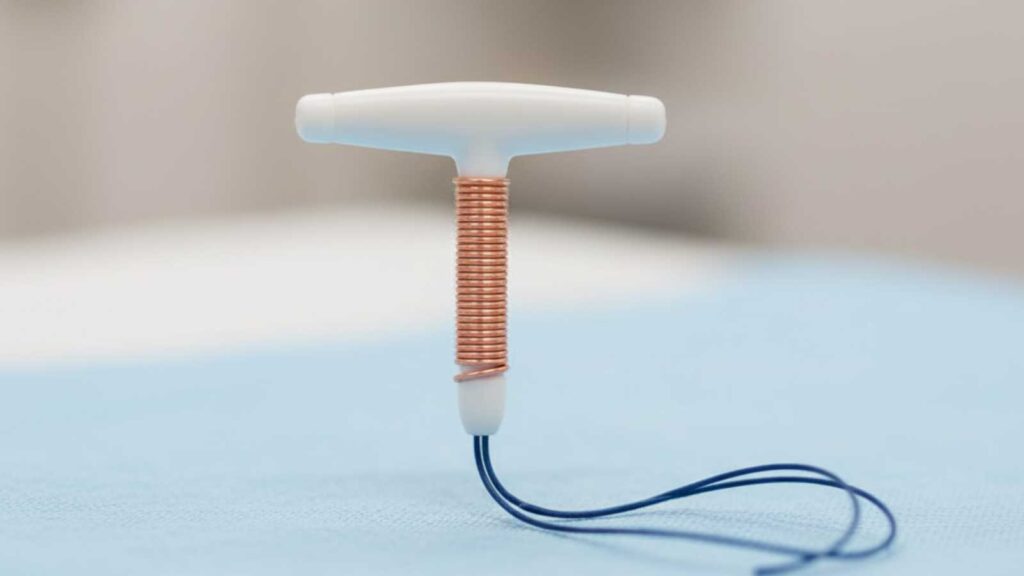
This small, T-shaped device works silently in the background of your life, providing continuous protection while you focus on what matters most. Modern IUDs have undergone significant evolution since their earlier versions, incorporating advanced materials and enhanced insertion techniques that make them safer and more comfortable than ever before.
Understanding Intrauterine Device Basics
An IUD measures approximately 1.25 inches long and fits comfortably inside your uterus, using multiple mechanisms that work together for maximum effectiveness. Your gynecologist inserts this device through your cervix during a brief office procedure, similar to getting a Pap smear, although the insertion process takes slightly longer. The device’s unique T-shape allows it to sit securely in your uterine cavity, with flexible arms that gently conform to your body’s natural contours.
The pregnancy prevention mechanism works primarily by creating an environment that prevents sperm from reaching and fertilizing an egg, rather than terminating an existing pregnancy. This occurs through changes in cervical mucus consistency, alterations in the uterine lining, and, in some cases, the prevention of ovulation, depending on the IUD type you choose.
Two Main IUD Types Available
IUDs come in two distinct types, hormonal and copper, each offering unique benefits to match your contraceptive preferences and health needs.
Key differences between IUD types:
- Hormonal IUDs release a steady, low dose of progestin directly into your uterus, providing localized hormone delivery that minimizes systemic side effects
- These devices typically last between three to six years and often result in lighter, less painful periods
- Copper IUDs contain no hormones whatsoever, making them ideal if you prefer hormone-free contraception or have medical conditions that contraindicate hormonal methods
- The copper wire creates a natural spermicidal environment that prevents fertilization for up to 10 years.
- Copper IUDs represent the longest-acting reversible contraceptive option available
Your gynecologist can help you choose between hormonal and copper IUDs based on your individual health profile, lifestyle needs, and contraceptive goals.
ALSO READ: Best Birth Control Options for Women Over 35
IUD Benefits and Key Advantages
The remarkable effectiveness and convenience of IUDs make them an attractive option for women seeking reliable birth control without the daily commitment required by other methods. You gain the freedom to live your life without constantly thinking about contraception, while enjoying protection rates that rival permanent sterilization procedures but remain completely reversible. These advantages extend beyond simple pregnancy prevention, offering additional health benefits that can improve your overall quality of life and menstrual experience.
Exceptional Effectiveness and Longevity
IUDs prevent pregnancy with exceptional reliability, making them more effective than birth control pills, condoms, or other commonly used contraceptive methods you might have tried previously. This superior effectiveness rate gives you confidence in your chosen protection method, allowing you to plan your future with certainty. The reversible nature of IUDs provides peace of mind if your family planning goals change, as fertility typically returns to baseline levels within months of removal.
Hormonal IUDs function effectively for three to six years, depending on the specific type, while copper IUDs can protect you for a decade. This longevity eliminates the worry of running out of birth control or missing appointments for prescription renewals, particularly important if you have irregular schedules or limited access to healthcare services.
Convenience and Lifestyle Benefits
Once your OBGYN inserts your IUD, you can essentially forget about birth control for years while maintaining complete protection against unintended pregnancy. This convenience proves especially valuable for women with busy lifestyles, irregular schedules, or difficulty remembering daily medications that other contraceptive methods require. The device remains completely invisible to you and your partner during intimacy, allowing for spontaneous moments without contraceptive interruption.
Breastfeeding mothers benefit significantly because hormonal IUDs contain only progestin, avoiding estrogen that could interfere with milk production or quality. This makes IUDs an excellent choice for postpartum contraception, particularly if you’re planning to breastfeed for an extended period but want reliable birth control protection.
Menstrual and Health Benefits
Hormonal IUDs often transform your menstrual experience, providing lighter, shorter, and less painful periods that can dramatically improve your quality of life each month.
Key menstrual and health advantages:
- Significant reduction in menstrual flow, with some users seeing their periods stop completely after the first year
- Particularly beneficial if you suffer from heavy periods, anemia, or conditions like endometriosis that cause severe cramping
- Copper IUDs may potentially protect against cervical cancer
- Fertility returns quickly after IUD removal, typically within a few months, allowing you to conceive when you’re ready
These benefits extend beyond contraception alone, making IUDs a valuable option for managing menstrual symptoms and supporting your overall reproductive health without long waiting periods when you decide to start a family.
Cost-Effective Long-Term Solution
The upfront cost of an IUD insertion may seem significant, but when calculated over the device’s lifespan, it becomes one of the most economical contraceptive choices available to you. Most insurance plans cover IUD insertion and the device itself under preventive care provisions, potentially eliminating out-of-pocket costs. Even without insurance coverage, the total cost over three to ten years often equals less than what you’d spend on birth control pills, condoms, or other monthly contraceptive expenses.
This economic advantage becomes even more pronounced when you factor in the reduced need for OBGYN visits related to contraceptive management, prescription refills, and potential costs associated with unintended pregnancies.
Potential Risks and Side Effects
While IUDs offer exceptional safety profiles for most women, understanding potential risks and side effects helps you make an informed decision and know what to expect during your contraceptive experience. Most side effects remain mild and temporary, resolving within the first few months as your body adjusts to the device. Your gynecologist can help you weigh these potential concerns against the significant benefits IUDs provide, ensuring you choose the option that best fits your individual health profile and lifestyle needs.
Insertion Process and Discomfort
The IUD insertion procedure occurs in your OBGYN office and typically takes less than five minutes, though some women experience cramping during and immediately after the process similar to strong menstrual cramps. Your healthcare provider may recommend taking over-the-counter pain medication before your appointment to minimize discomfort. Most women return to normal activities immediately, though avoiding heavy lifting for 24 hours is recommended.
Hormonal IUD Side Effects
Irregular bleeding patterns represent the most common side effect during the first three to six months, including light spotting between periods or unpredictable timing that gradually stabilizes. Some women experience mild side effects such as breast tenderness, headaches, or mood changes, though the low-dose, localized hormone delivery usually produces fewer systemic effects than oral contraceptives.
Copper IUD Considerations
Copper IUDs may increase menstrual flow and cramping, particularly during the first few months after insertion, though these changes typically improve over time. Women with copper allergies or Wilson disease cannot use copper IUDs and should choose hormonal IUDs instead.
Rare but Serious Complications
IUD expulsion occurs occasionally, typically within the first year after insertion, and requires immediate replacement if you want to maintain contraceptive protection. Signs of expulsion include feeling the IUD strings protruding at your cervix, increased cramping, or unusual bleeding patterns that prompt evaluation by your gynecologist. Regular check-ups help detect expulsion early and ensure continued protection.
Uterine perforation during insertion remains extremely rare and typically gets detected and managed immediately by your experienced OBGYN provider. While IUDs provide excellent pregnancy prevention, they don’t protect against sexually transmitted infections, so you’ll need barrier methods like condoms if STI protection is essential for your sexual health.
Common IUD Myths Debunked
Misconceptions about IUD safety and effectiveness persist despite decades of research proving their benefits, often stemming back to outdated information about older devices that were removed from the market decades ago.
You deserve accurate, current information based on modern research and clinical experience rather than fears rooted in historical problems that no longer apply to today’s devices. Understanding the facts helps you make decisions based on evidence rather than anxiety-provoking myths that may prevent you from accessing excellent contraceptive options.
Safety and Fertility Misconceptions
Modern IUDs bear little resemblance to the problematic Dalkon Shield from the 1970s that created lasting but unfounded fears about IUD safety and fertility effects.
Key facts about IUD safety and fertility:
- Current devices undergo rigorous testing and regulatory approval processes, with millions of women worldwide using them safely for decades
- Fertility returns to normal baseline levels after IUD removal, regardless of how long you’ve used the device
- IUD use doesn’t increase your risk of infertility, ectopic pregnancy, or pelvic inflammatory disease when inserted under proper medical conditions
- Pregnancy rates after IUD removal are comparable to women who never used IUDs
Your gynecologist can provide reassurance based on extensive clinical data showing that modern IUDs are both safe and fully reversible contraceptive options.
Pregnancy and Abortion Myths
Understanding how IUDs actually work helps address common misconceptions about their mechanism of action and relationship to pregnancy.
Key facts about IUDs and pregnancy:
- IUDs prevent pregnancy primarily by preventing fertilization from occurring, not by terminating established pregnancies
- The device creates an environment hostile to sperm survival and egg fertilization, working before conception rather than after implantation
- IUDs actually reduce your overall ectopic pregnancy risk compared to using no contraception at all, due to their exceptional effectiveness at preventing all pregnancies
These facts address concerns some women have about the moral implications of IUD use and clarify how the device functions as a preventive contraceptive method.
Candidacy and Age Myths
Medical research has thoroughly debunked outdated beliefs about who can safely use IUDs, expanding access to women of all ages and reproductive histories.
Key facts about IUD candidacy:
- Women who haven’t given birth (nulliparous women) can safely use IUDs with insertion techniques adapted for smaller cervical openings
- Age restrictions have been proven unnecessary, with both adolescents and women approaching menopause benefiting from IUD use
- Medical appropriateness depends on individual health profiles, not pregnancy history or age alone
When medically appropriate for your individual health profile, IUDs offer safe and effective contraception regardless of whether you’ve had children or where you are in your reproductive years.
Infection and Weight Concerns
Understanding the facts about infection risk and weight changes helps dispel common myths about IUD use and allows you to make informed decisions about your contraceptive choice.
Common concerns include:
- Infection rates following IUD insertion remain extremely low, occurring primarily within the first few weeks when proper sterile technique is followed
- The risk equals that of other gynecological procedures and doesn’t increase with long-term IUD use
- Most studies find no difference between IUD users and non-users over time regarding weight
- Localized hormone delivery produces fewer systemic effects than oral contraceptives
Your healthcare provider follows strict protocols to minimize infection risk and will guide you through post-insertion care to optimize healing and address any concerns you may have.
ALSO READ: Annual Well-Woman Exam: What’s Included and Why It Matters
Is an IUD Right for You?
Your gynecologist evaluates your lifestyle, health history, and contraception goals to determine if an IUD suits your needs. This decision strikes a balance between effective pregnancy prevention and your preferences regarding hormones, menstrual changes, and maintenance requirements, taking into account your individual risk factors.
Ideal Candidate Characteristics
IUDs are most effective for long-term protection, eliminating the need for daily maintenance, prescription refills, or frequent OBGYN visits. You benefit most if you seek three-plus years of consistent protection, have difficulty remembering daily medications, travel frequently, or prefer minimal healthcare appointments. Hormonal IUDs suit women wanting lighter periods, while copper IUDs appeal to those avoiding hormones altogether.
Medical and Lifestyle Factors
Your health history determines IUD suitability, especially if you have hormone-sensitive conditions, bleeding disorders, or anatomical variations affecting insertion. Certain medications reduce hormonal contraceptive effectiveness, making copper IUDs preferable. Your provider reviews your complete medical history, including previous high-risk pregnancy situations affecting your choice.
STI risk based on relationship status and sexual practices matters since IUDs don’t provide the infection protection that barrier methods offer.
Making an Informed Decision
Consultation with your gynecologist provides a personalized risk-benefit analysis that considers your specific health profile, lifestyle needs, and reproductive goals rather than generic population-based recommendations.
This individualized approach helps identify which IUD type aligns best with your preferences about hormones, menstrual changes, and the duration of protection you desire. Your provider can address specific concerns, review your complete medical history, and discuss how IUDs compare to other contraceptive options you’re considering.
The decision-making process should include discussion of your timeline for potential pregnancy, career considerations, relationship factors, and any medical conditions that might influence your contraceptive choice or require special monitoring.
Next Steps at Gwinnett OB/GYN
Gwinnett OB/GYN’s experienced providers offer comprehensive contraceptive counseling that includes a thorough evaluation of your medical history, a discussion of all available options, and personalized recommendations tailored to your individual needs and preferences.
The consultation process includes a detailed explanation of insertion procedures, expected experiences, and follow-up care protocols that ensure your comfort and safety throughout your IUD experience. Our board-certified physicians and nurse practitioners stay current with the latest advances in women’s healthcare, providing you with evidence-based guidance for your contraceptive decisions.
Schedule your consultation today to discuss if an IUD aligns with your reproductive health goals and lifestyle needs. Contact Gwinnett OB/GYN to begin your personalized contraceptive evaluation and take the first step toward long-term birth control that fits seamlessly into your life.